Healthcare, Grief, and Personal Wellness
Physiological and Emotional Regulation in Healthcare

High-stress environments can intensify grief, increasing both its emotional impact and how frequently it surfaces. In addition to grief-specific coping tools, strategies that support general stress management may play an important role in sustaining emotional well-being.
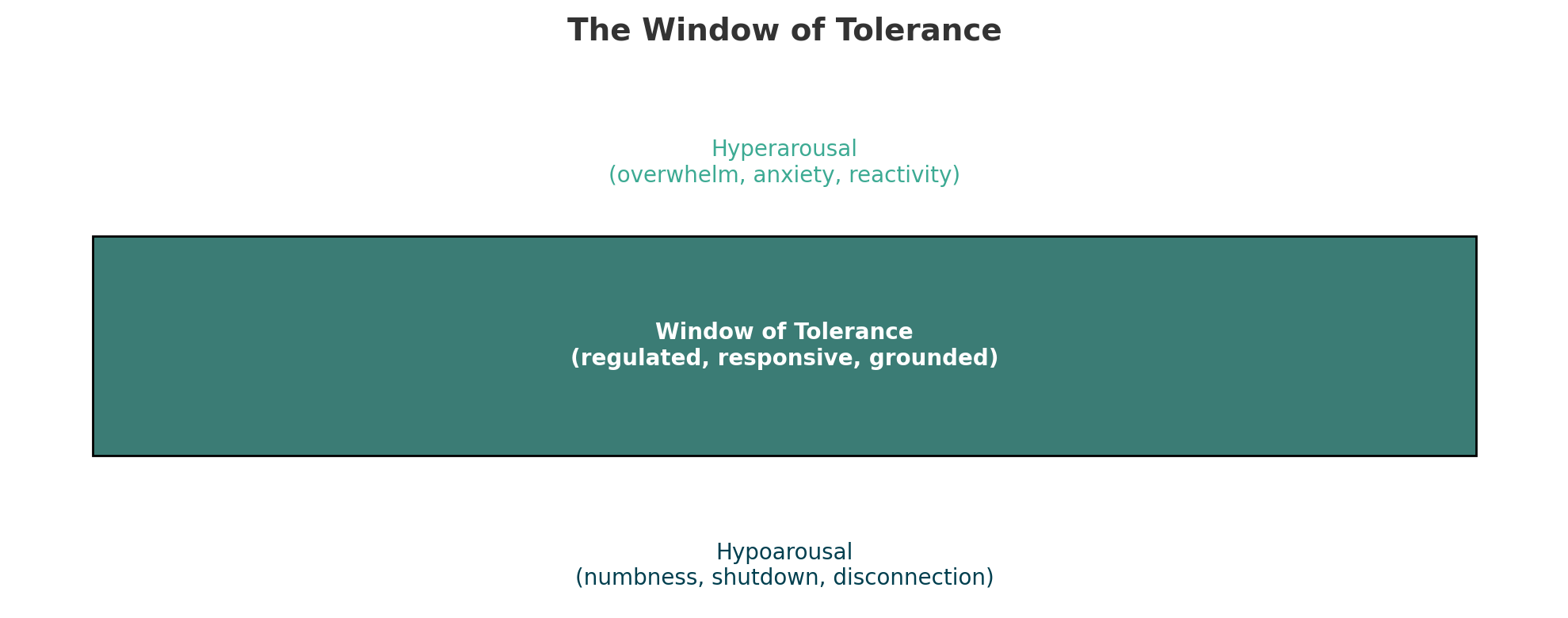
The Window of Tolerance
The Window of Tolerance, a concept developed by psychiatrist Dr. Daniel Siegel, refers to the range of emotional functioning in which individuals are most able to think clearly, remain grounded, and respond in ways that align with their values, even under stress.
Grief, trauma, and cumulative distress may narrow this window, increasing the likelihood of moving outside of it, including:
- Hyperarousal — Feeling anxious, overwhelmed, emotionally flooded, or reactive
- Hypoarousal — Feeling numb, shut down, disconnected, or disengaged
Indicators of Dysregulation
Hyperarousal, such as overwhelm, anxiety, or reactivity, may occur after sudden patient deaths, multiple losses in a single shift, unexpected reactions from grieving supporters, or traumatic codes that do not result in survival.
Hypoarousal, such as numbness, withdrawal, or disconnection, may show up after repeated losses, during end-of-life care that begins to feel automatic, during emotional shutdown in team settings, or as a sense of exhaustion and disconnection without a clear cause.
Strategies for Regulation
Evidence-based regulation strategies can support a return to the window of tolerance when stress or grief pushes regulation beyond it. Coping strategies can support regulation through multiple pathways, including, physiological, cognitive, emotional, and behavioral processes.
Physiological
Physiological regulation strategies that directly support nervous system regulation and body-based calming.
Breath is the bridge which... unites your body to thoughts. Whenever your mind becomes scattered, use your breath as the means to take hold of your mind again.

Breathwork
Breathwork refers to the intentional use of breathing patterns to support nervous system regulation. Even brief periods of slow, controlled breathing can support a shift toward calmer physiological states, helping promote emotional steadiness and clearer thinking during moments of stress, grief, or trauma exposure in care settings.
Breathwork Exercises to Try
Physiological Sigh
A brief breathing pattern used to support rapid down-regulation of acute physiological arousal.
How to do it: Take a deep inhale, followed by a second short sip of air. Exhale slowly through the mouth. Repeat 1–3 times.
Why it can help: Prolonged exhalation and lung inflation patterns can support rapid calming of stress responses.
Slow Paced Breathing (Extended Exhale)
A slow breathing pattern that emphasizes a longer exhale to support parasympathetic activation.
How to do it: Inhale through the nose for 4 seconds → exhale slowly for 6 seconds. Repeat for 1–3 minutes.
- Why it can help: Slower breathing with extended exhalation can support calming physiological responses and improved emotional regulation.
Grounding
Grounding techniques are evidence-informed strategies that use sensory and cognitive input to support nervous system regulation and re-establish present-moment awareness. In high-stress or emotionally charged situations, grounding can help interrupt escalation, reduce disengagement or dissociation, and support functional engagement, which can help maintain clinical effectiveness and emotional steadiness.
Grounding Practices to Try
Touchpoint Anchoring
- Touchpoint anchoring is a sensory-based grounding strategy that uses physical contact to support present-moment awareness and nervous system regulation.
- How to do it:
- Grip a cold water bottle or press hands onto a cool surface (a metal tray, sink).
- Run fingers along a textured object (badge lanyard, pen cap, scrub pocket seam).
- Press feet into the floor and notice contact from heel to toe.
- Why it can help: Tactile and temperature input engage somatosensory pathways, which can help shift attention from distressing internal experiences to physical cues in the present moment, supporting re-orientation and regulation.
5-4-3-2-1 Sensory Grounding
- The 5-4-3-2-1 technique is a structured, multisensory grounding exercise used to support present-moment orientation during acute stress or emotional overload.
- How to do it: Silently observe and name:
- 5 things that can be seen
- 4 things that can be touched
- 3 things that can be heard
- 2 things that can be smelled
- 1 thing that can be tasted
- Why it can help: Engaging multiple senses can redirect attention to the external environment, support interruption of dissociation or emotional flooding, and promote functional engagement in the present moment.
Wall Grounding (Proprioceptive Support)
- Wall grounding is a sensory-based regulation strategy that uses firm physical contact with a stable surface to support present-moment awareness and nervous system regulation.
- How to do it:
- Stand with the back, shoulders, or hips against a wall.
- Press feet firmly into the floor and notice points of contact.
- Gently press the body into the wall for 30–60 seconds while maintaining slow, steady breathing.
- Why it can help: Proprioceptive and tactile input from firm contact can increase body awareness and support down-regulation of emotional arousal by engaging somatosensory pathways, consistent with trauma-informed and somatic approaches
Dissociation is a protective response in which attention, awareness, or emotional experience becomes partially disconnected from overwhelming thoughts, emotions, or sensations. It can present as numbness, detachment, mental fog, or a sense of functioning on autopilot.
In healthcare settings, dissociation can support short-term functioning during highly stressful or overwhelming events. Over time, persistent dissociation can indicate cumulative stress and a need for additional support, rest, or opportunities to process emotionally demanding experiences.
Micro-Movements
- Micro-movements are small, intentional physical adjustments that can support nervous system regulation and release physical tension without disrupting clinical workflow.
- How to do it:
- Gently roll shoulders or stretch the neck side to side.
- Shift weight from one foot to the other while standing.
- Subtly wiggle toes inside shoes.
- Why it can help: Brief, low-intensity movement can support discharge of physical tension and reduce somatic signs of hyperarousal, while remaining feasible within clinical environments.

Bilateral and Rhythmic Movements
Bilateral and rhythmic movements involve simple, repetitive actions that engage both sides of the body. These movements can support nervous system regulation by providing predictable sensory and motor input, which can help reduce physiological arousal and support emotional steadiness after stress or distress.
How to do it:
Alternating hand taps on thighs or crossed arms (left–right–left)
Gentle side-to-side rocking or swaying while seated or standing
- Alternating hand movements such as light drumming on legs
- Why it can help: Body-based and rhythmic strategies provide structured sensory input that can support regulation by engaging sensorimotor pathways and promoting a sense of predictability and safety.
Cognitive
Cognitive strategies that support how thoughts and meaning are processed.
Internal Reorientation
- Internal reorientation uses simple cognitive and contextual cues to support present-moment awareness and a sense of safety during emotional or cognitive overload. These strategies can be especially helpful when stress, grief, or trauma exposure contributes to dissociation, anxiety, or emotional flooding.
- How to do it:
- Silently repeat a grounding phrase (for example, “I am here. This is now. I am safe enough.”).
- Name the date, time, and current location (for example, “It’s Tuesday. I’m in the break room. I have 10 minutes left.”).
- Why it can help: Re-establishing orientation to time, place, and context can support interruption of dissociation and emotional flooding by engaging cortical awareness and reinforcing present-moment safety.
Cognitive Reframing
- Cognitive reframing involves intentionally examining and shifting how a situation is interpreted, without dismissing pain or difficulty. This approach can support emotional regulation by helping maintain connection to meaning, agency, and purpose in the context of challenging clinical experiences.
- How to do it: Shift internal statements, for example:
- “I failed.” → “I showed up, provided care, and did the best I could with what was possible.”
- “I should have caught that sooner.” → “I acted on the information available at the time and followed appropriate clinical processes.”
- “I should be able to handle this by now.” → “Ongoing exposure to loss can affect anyone, regardless of experience.”
- Why it can help: Cognitive reframing can reduce shame, rumination, and helplessness by shifting internal narratives. This can support a sense of efficacy, preserve empathy, and help healthcare professionals navigate morally complex situations without internalizing systemic limitations.
Research from the Penn State Nese College of Nursing shows that brief, structured strategies like reframing, self-talk, and goal setting can support lasting emotion regulation.
Participants with the highest distress saw the greatest improvement. One year later, 96 percent still used at least one skill weekly. The most common strategies were positive thinking and self-talk.
Self-compassion
Self-compassion means offering yourself the same care you would give to others. It supports emotional regulation, resilience, and recovery from distress. In clinical environments, it can serve as a protective factor against burnout.
How to do it: Shift your self-talk:
After getting short with a resident during a long, understaffed shift: “I should have been more patient.” → “Fatigue and workload strain affect communication. This reflects system pressure, not lack of care or professionalism.”
After a difficult family interaction: "I handled that badly.” → “That was a complex, emotional situation. I did my best to stay present and respectful.”
After a patient death: “I should be stronger than this.” → “Being affected reflects connection, not weakness.”
Why it works: Research suggests that higher levels of self-compassion are associated with lower emotional exhaustion and depersonalization among healthcare professionals, indicating that self-compassion can function as a protective factor against burnout.
When self-compassion feels difficult, pausing to observe and name internal experience can be a first step. For example, “I’m noticing self-critical thoughts right now.” This type of mindful awareness can support reduced reactivity and create space for more supportive internal responses.
To explore emotional and behavioral coping strategies, access the GSHP resource on Sustained Strategies for Personal Wellness.

Staying Regulated in Grief-Exposed Care
Regulation is a clinical skill that supports both emotional well-being and sustained capacity to provide care. The strategies in this section offer practical ways to restore steadiness when grief and stress push regulation outside the window of tolerance. Over time, intentional and consistent use of coping strategies can support resilience, preserve emotional presence, and reduce the cumulative impact of grief-exposed care.